Recognizing the Critical Signs of Dry Socket - What You Need to Know After Wisdom Teeth Extraction
After a tooth extraction, many patients expect some discomfort and swelling, but understanding the signs of dry socket is crucial for timely intervention. Dry socket is a painful complication that occurs when the blood clot at the extraction site becomes dislodged or dissolves prematurely, exposing underlying nerve endings and bone. Recognizing these signs early can be life-changing, helping you seek prompt dental care and avoid further complications.
In this comprehensive article, we will delve into the signs of dry socket, explore how you can identify if you have dry socket, what dry socket looks like, and discuss post-operative symptoms to watch for following tooth extraction. We will also provide insights into the early-stage symptoms and when symptoms typically start, empowering you to take proactive steps for your dental health.
Signs of dry socket
After an extraction, the presence of a dry socket can significantly affect your recovery process. Understanding its signs of dry socket is essential to distinguish normal healing discomfort from a more serious complication. Typically, dry socket manifests with specific symptoms that usually appear within a few days after surgery.
Dry socket signs include intense pain at the extraction site, which often radiates to the ear, eye, or neck on the same side. The pain tends to be disproportionate to the typical healing process and does not subside with commonly used pain relievers. Additionally, there may be a foul taste or bad breath, a visible empty socket where the blood clot should remain, and sometimes, exposed bone that can be tender when touched.
A patient might also notice swelling around the extraction site, or the area may appear dry and devoid of the normal blood clot that facilitates healing. The absence of a blood clot or the presence of a canker sore-like lesion are strong indicators of dry socket. Recognizing these signs of dry socket early provides a critical window for seeking treatment to alleviate pain and prevent infection.
Pain that is unrelieved by analgesics
One of the hallmark signs of dry socket is persistent and severe pain that does not respond to over-the-counter pain medications. Unlike typical post-extraction discomfort that gradually decreases, the pain associated with dry socket tends to worsen over time. Patients report a deep, throbbing ache that can extend to the ear, temple, or jaw, making it difficult to eat or speak comfortably.
This pain usually begins between the second and fourth day after the procedure. If you notice that the prescribed painkillers are ineffective or only temporarily provide relief, it might be a sign that something more serious, like dry socket, is happening. It’s vital to communicate these symptoms to your dentist promptly, as they can suggest appropriate interventions such as medicated dressings or antibiotics.
Visible evidence of an empty socket
Neurological and visual cues are often the most direct signs of dry socket. On inspection, you might notice an empty socket where the blood clot has been lost, replaced by exposed bone or tissue. This is a clear indication that the healing process is compromised.
The socket may look devoid of the usual dark, clot-like material, appearing more like a pink or white barren cavity. Sometimes, you might see fragments of bone or a crust of tissue covering the area. Patients often describe this as a hollow or raw appearance that is painful to touch. Proper assessment by a healthcare professional is essential to confirm whether the dry socket is present or if other issues, such as infection, are involved.
Symptoms that extend beyond typical healing
While mild discomfort and swelling are normal in the first few days after pulling a tooth, certain symptoms should raise concern. These include a persistent bad taste or foul odor emanating from the extraction site, indicating infection or tissue necrosis linked with dry socket. Also, if swelling continues to increase instead of decreasing, or if fever develops, these could be signs of dry socket or associated complications.
Monitoring these symptoms closely is vital because they can lead to secondary infections or delayed healing. Patients should be aware that dry socket rarely occurs without other signs, so if your pain and symptoms persist or worsen, prompt consultation with your dentist becomes necessary to prevent further complications.
How do you know if you have dry socket
Determining how do you know if you have dry socket can be challenging for those unfamiliar with post-extraction symptoms. However, awareness of the characteristic signs of dry socket and understanding the typical timeline aids in earlier diagnosis and intervention.
Most cases of dry socket develop between 2-4 days after extraction, though this can vary based on individual healing. Recognizing early indications such as severe pain, foul taste, and observable empty socket features are essential in differentiating dry socket from normal post-operative discomfort.
The key factors to consider include the intensity and progression of the pain, the appearance of the socket, and accompanying symptoms like bad breath or swelling. Patients often report that the pain feels deep, throbbing, and unrelieved by analgesics, which is a significant indicator. Additionally, the absence of the blood clot or evidence of exposed bone are clinical signs that your oral tissue may be suffering from dry socket.
Differentiating dry socket from normal healing
Post-extraction discomfort typically peaks around the third day but gradually subsides afterward. If pain persists beyond this period or intensifies rather than diminishes, it could signify dry socket. Moreover, the presence of visible signs such as an empty socket or exposed bone strongly suggests abnormal healing.
Patients often ask, "how do you know if you have dry socket?" One reliable method involves assessing the timing, intensity, and specific signs of dry socket like bad taste, bad smell, or raw appearance of the extraction site. Consulting your dentist to confirm these observations helps in initiating appropriate treatment—such as medicated dressings or antibiotics—which can significantly reduce pain and promote healing.
Personal experiences and criteria for diagnosis
Many patients have described the pain as throbbing and intense, often out of proportion to typical post-surgical discomfort. Personal accounts reinforce the importance of paying attention to changes during healing, especially if pain seems disconnected from expected recovery timelines.
Clinically, diagnosis involves a thorough dental examination, including inspection of the socket. Dentists look for classic signs like absence of clot, exposed bone, or a foul odor. Radiographs may sometimes be used to rule out secondary infection or other complications. Understanding how do you know if you have dry socket allows patients to seek timely intervention and reduce discomfort.
When in doubt, consult your dentist
It’s crucial to remember that only a qualified dental professional can definitively diagnose dry socket. Patient awareness and attentiveness to symptoms are vital, as early detection significantly improves treatment outcomes. If you experience any strong or unusual symptoms around the extraction site, consult your dentist promptly.
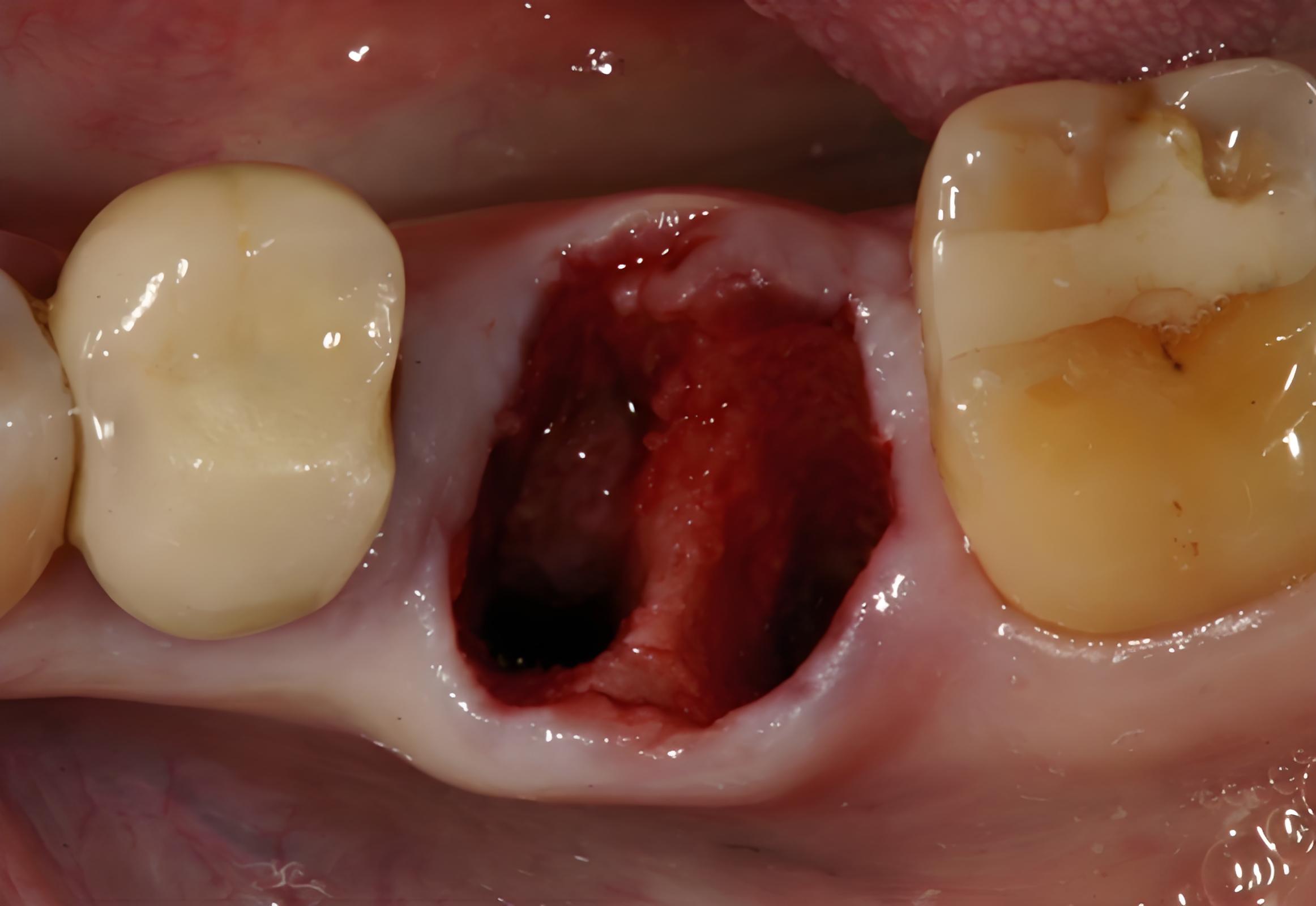
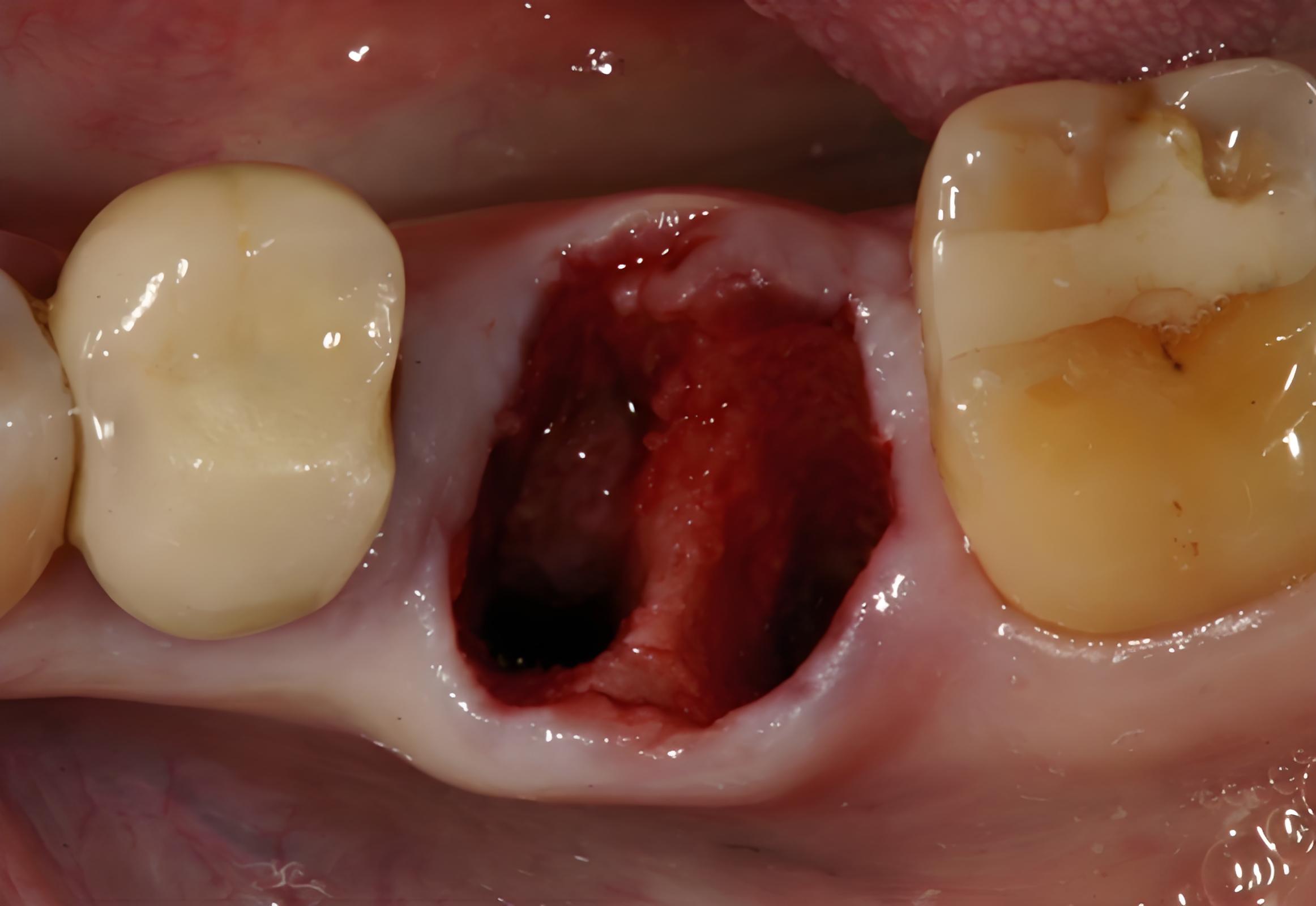
What does dry socket look like
Knowing what does dry socket look like helps in visually recognizing the complication and seeking timely care. Visual cues are often the most concrete evidence of dry socket, especially when you observe the extraction site directly or during a post-operative check-up.
Dry socket appears as a dry, empty socket often devoid of the usual blood clot. Instead of a dark, gel-like clot, the socket may look pale or white, with visible bone or nerve tissue. Sometimes, fragments of bone can be seen, and the area may be sensitive or painful upon touch.
The clarity of this visual presentation enables patients and practitioners to distinguish dry socket from normal healing sites. While some swelling and discomfort are expected, these specific visual signs tend to indicate abnormal healing conditions that require medical attention.
Visual differences between normal and dry socket healing
In normal healing, the extraction site should gradually fill with new tissue, forming a blood clot, which then gets replaced by granulation tissue and eventually new bone. The socket transitions from a dark, blood-filled cavity to a pink, closed wound.
In contrast, what does dry socket look like is characterized by an open, empty cavity often with exposed bone, as the clot has been lost. The site may appear raw, with visible bone fragments or tissue. This stark visual difference signifies that healing has been disrupted, necessitating professional care. Recognizing these signs early can prevent further complications.
Contributing factors influencing visual appearance
Certain behaviors or circumstances can influence what dry socket looks like. For example, smoking or vigorous rinsing may dislodge the blood clot prematurely, resulting in a more pronounced dry socket appearance. Nutritional deficiencies or systemic health issues might also impair normal healing, leading to abnormal visual signs.
Understanding these factors can help patients adopt preventative measures and identify early deviations from normal healing. If you visually notice an empty cavity with exposed bone, especially coupled with pain, seek dental assistance without delay.
Case studies and real-life examples
Many dental case studies and patient reports reinforce the visual cues associated with dry socket. For instance, patients mention the absence of the expected dark clot and the presence of a "raw, empty" cavity with or without exposed bone.
These visual cues, combined with symptoms like pain and foul taste, form a comprehensive picture that guides diagnosis. Being familiar with what does dry socket look like directly influences prompt treatment and faster recovery.
Dry socket after tooth extraction
Understanding the dry socket after tooth extraction involves recognizing how and why it occurs, and preparing for possible complications. Although it's a common concern, most dry sockets are preventable with proper post-operative care and patient compliance.
The condition often develops when the blood clot, necessary for healing, is dislodged or dissolves prematurely. This results in the exposed bone and nerve endings becoming vulnerable to bacterial invasion and environmental factors.
The timeframe for dry socket after tooth extraction generally falls between two to five days, making awareness during this window crucial. Patients often ask about their risk and how to minimize it through diligent care and precautions.
Risk factors associated with dry socket after extraction
Certain factors increase the likelihood of developing dry socket after tooth extraction. These include smoking, poor oral hygiene, traumatic extractions, oral contraceptive use, and systemic diseases like diabetes. Patients with a history of dry socket are also at risk of recurring it in subsequent procedures.
Understanding these contributors helps tailor preventive strategies. For example, smoking and vigorous rinsing are often discouraged during healing, promoting clot stability and reducing dry socket occurrence.
Prevention strategies and patient advice
The best way to mitigate dry socket after tooth extraction involves pre- and post-operative care. Shrinking your risk can include avoiding smoking, using prescribed medications properly, maintaining excellent oral hygiene, and following your dentist’s instructions precisely.
Patients should be advised to rest, avoid spitting or rinsing vigorously, and stick to a soft diet during the initial healing phase. Proper hydration and nutrition also contribute to optimal healing and clot stability.
Typical progression and healing timeline
The healing process after tooth extraction usually proceeds smoothly, with tissue regeneration gradually replacing the blood clot. However, if the blood clot is lost prematurely, dry socket symptoms set in, affecting healing.
Most cases necessitate medical intervention to manage pain and promote healing. Knowledge of the dry socket after tooth extraction timeline and symptoms allows patients to seek care promptly and minimize discomfort and complications.
Data table: Risk Factors for Dry Socket
| Risk Factor | Percentage of Cases | Description |
|---|---|---|
| Smoking | 30% | Increases risk by disrupting blood clot formation |
| Poor oral hygiene | 25% | Leads to bacteria proliferation, interfering with healing |
| Traumatic extraction | 20% | Excessive force may dislodge the clot |
| Oral contraceptives | 15% | Hormonal influence may impair clot stability |
| Systemic diseases | 10% | Conditions like diabetes compromise healing |
(Note: percentages are estimates based on clinical observations)
Early stage dry socket symptoms
Recognizing early stage dry socket symptoms enables timely intervention, reducing pain and preventing infection. These early signs are often subtle but can escalate quickly if ignored.
Patients typically notice discomfort starting around the second or third day after extraction, characterized by increasing pain localized at the site. The pain may intensify, feeling throbbing and deep, not responding well to pain medication. Swelling around the site might also develop.
Other early signs can include a noticeable foul taste or odor, suggesting bacterial activity. The socket may still appear mostly intact, but tenderness and sensitivity are common. Patients are advised to monitor these symptoms closely during the initial healing period.
Symptoms preceding full dry socket
Before dry socket fully develops, patients may experience initial indicators such as mild swelling, slight discomfort, or an unusual sensation at the extraction site. Recognizing these early symptoms allows patients to alert their dentist before the condition worsens.
The transition from normal healing discomfort to early dry socket symptoms often involves a shift in pain quality—becoming sharper or more persistent. Addressing these early signs can prevent the progression to more severe, full-blown dry socket.
Additional signs to watch out for
Apart from pain, other early symptoms include bad taste, bad breath, or mild swelling around the surgical area. Patients may also notice that analgesics are becoming less effective. These signs should prompt a dental consultation to evaluate the site and prevent escalation.
Close attention to oral hygiene and avoiding habits like smoking can mitigate the severity of early symptoms. Recognizing and managing early stage dry socket symptoms is key to a smoother recovery process.
Personal experiences of early symptoms
Patients commonly describe initial pain as a dull ache that worsens suddenly. Many report that pain medication no longer alleviates the discomfort, raising concern. Some notice small changes in the appearance of the site, like slight redness or tenderness.
Understanding these early cues helps in seeking urgent dental advice. Early intervention often involves medicated dressings or rinses that can significantly reduce the severity and duration of dry socket.
When do dry socket symptoms start
Knowing when do dry socket symptoms start is fundamental for patients who want to monitor their healing and act quickly if problems arise. Most symptoms typically develop within a specific time window post-extraction, helping clinicians and patients plan for potential complications.
In general, symptoms of dry socket usually begin between the second and fifth day after the procedure. This timing aligns with the normal timeline for clot dislodgment or dissolution. Patients should be particularly vigilant during this period if they experience disproportionate pain, foul taste, or abnormal appearance at the site.
Typical timeline for symptom onset
The onset of signs of dry socket can vary depending on individual healing, type of extraction, and adherence to postoperative care. For most patients, symptoms are noticeable around day 3-4, with peak pain often occurring between days 3-5.
Monitoring the extraction site closely during this critical period aids in early detection. If symptoms develop earlier or later than the expected window, consulting your dentist can help uncover underlying causes and appropriate treatment.
Factors influencing onset timing
Factors such as smoking, trauma during extraction, and systemic health influence when symptoms start. Patients with compromised healing or poor oral hygiene may experience symptoms earlier or more intensely.
Moreover, some individuals may be asymptomatic initially, experiencing only mild discomfort that suddenly intensifies. This variability underscores the importance of awareness and regular check-ups following extraction procedures.
Personal case reports
Many patients have reported symptoms starting specifically around day 3 or 4 post-extraction. Descriptions often include sudden severe pain, foul taste, and exposed bone, consistent with signs of dry socket manifesting. Recognizing these patterns helps in prompt diagnosis and management.
In conclusion, understanding when do dry socket symptoms start equips you with expectations for the recovery timeline and emphasizes the importance of vigilant postoperative care.
FAQs
Q1: What are the main signs of dry socket I should look for after tooth extraction? A: The primary signs of dry socket include severe pain that worsens over time, an empty socket with exposed bone, foul taste or odor, swelling, and sometimes a visible lack of blood clot at the extraction site.
Q2: How do you know if you have dry socket early on? A: How do you know if you have dry socket early is often through increasing pain around days 2-4 after extraction, along with bad taste, tenderness, and visible empty socket. Prompt dentist consultation is advised for confirmation.
Q3: What does dry socket look like? A: What does dry socket look like is characterized by an open, empty cavity with exposed bone and tissue, often lacking the usual blood clot, and may feel raw or painful when touched.
Q4: When do dry socket symptoms typically start after tooth extraction? A: When do dry socket symptoms start usually occurs between the second and fifth day post-extraction, aligning with the time when the blood clot might dislodge.
Q5: Can you prevent dry socket? A: Yes, preventative measures include avoiding smoking, maintaining good oral hygiene, following post-operative instructions, avoiding vigorous rinsing or spitting, and taking prescribed medications as directed.
Conclusion
Understanding the signs of dry socket is vital for anyone recovering from tooth extraction, as early detection can significantly minimize pain and prevent secondary infections. The signs of dry socket like severe unrelieved pain, visible empty socket with exposed bone, foul taste, and swelling typically appear between days 2 and 5 after extraction. Recognizing how do you know if you have dry socket, especially through visual cues such as what dry socket looks like, and monitoring early symptoms can help you seek prompt treatment. Proper postoperative care and awareness of factors influencing dry socket after tooth extraction play crucial roles in healing. With timely intervention, many patients can manage this complication effectively, ensuring a smoother and less painful recovery process. Being informed and vigilant about when do dry socket symptoms start empowers you to prioritize your dental health and seek professional care at the right moment.





